29/F with polyarthritis and rashes
yesterday with complaints of loss of consciousness since 30 mins after alleged consumption of T.Clonazepam 2mg ( 2 tablets ) with hypoglycemia ( 56gm/dl)
Also complaints of polyarthritis since 4 months with morning stiffness in joints and pigmentation all over her face and ears since 3 months.
Seizures - 1st episode 4 years back (sudden tragic loss of sister being the trigger) used medication
2nd episode - after 6 months
3rd episode - after one year
4th episode - yesterday night ( lasted for 2 mins, post ictal confusion for 10 mins )
since April, 2022 she stopped taking T.PREDNISOLONE and T.HYDROXYCHLOROQUINE after discharge from hopsital
ICU bed no 4
Day 1
Unit 6
S: patient is responding to commands
C/o fever since 10 days
C/o oral ulcers
O: o/e patient is opening eyes on vocal commands
Patient is able to understand and able to recognise their attenders
Unable to speak making incoherent sounds
BP - 100/70 mmhg
PR - 110bpm
CVS - S1S2+
RS BAE+
P/A soft
Spo2 - 96% at Room air
She is having wincing of her face flexing her neck
Grbs - 60mg/dl at presentation after 25D --> 141 mg/dl
5pm - 83mg/dl
A: Altered sensorium secondary to Recurrent Hypoglycemia (?Adrenal insufficiency)
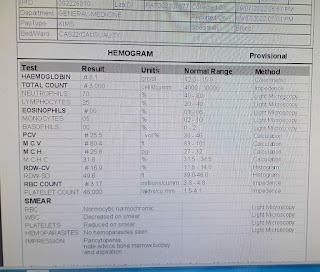
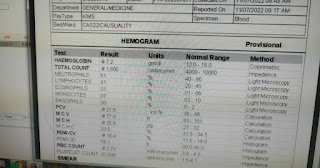
P: hemogram are awaited to rule out sepsis
RFT and LFT to rule out end organ damage
[09/07, 6:35 pm] Dr Rakesh Biswas Sir: @K vaishnavi mam gen med Inputs on her current problem
[09/07, 7:00 pm] shaileshpatil1996@gmail.com gen med: More detailed histiry admissions ?
Fever and other complaints ? Did she stop or missed her steroid dose ?
Unlikely to be adrenal insufficiency if someone is on 40 mg dose of prednisolone daily .
Let's wait for other investigations to rule out sepsis and renal involvement.
Did she have another episode of seizures recently?
Did her sensorium recover after 25D ?
If sensorium isn't improved yet ,could it be non convulsive status epilepticus or stroke . Would require complete neurological examination
Her GCS currently ?
[09/07, 7:29 pmhttps://shaileshpatil1996.blogspot.com/2022/07/29f-with-polyarthritis-and-rashes.html: She hasn't taking her steroid dose mam.. At time of presentation GCS E2V1M4 after 25D it's E4V2M6. As she is staying alone her daughter/mother is unable to give detailed elobrated timeline of events.. Reflexes are all intact 2+ mam with b/l plantars flexor response
Pupils B/L NSRL no episode of seizures as per their attenders history
[09/07, 7:35 pm] Dr Rakesh Biswas Sir: I think I have a word file about her that you shared. Check out the personal marital history in the link above, see the scalp hair and you may be able to recall
[09/07, 7:36 pm shaileshpatil1996@gmail.com: Okay since when did she stop steroids ? Although she isn't having hypotension currently ( which is also expected in case of adrenal insufficiency) .
After ruling out sepsis/ fever Would be better if you restart her on steroids
Why is she unable to speak ? Are there any other FND ?
[11/07, 8:40 am] Dr Rakesh Biswas Sir: How is her sensorium now? Is she still comatose?
@Dr. Rajkumar Could you recognize her?
If not I will tag the word file you had earlier shared about her again to you in pm
[11/07, 8:41 am] shaileshpatil1996@gmail.com: Her sensorium improved sir.. Responding to commands, no focal neurological deficits, E4V5M6 sir
[12/07, 9:46 am] Dr Rakesh Biswas Sir: Suggestive of sepsis
Her adrenal insufficiency could have been due to sepsis: @shaileshpatil1996@gmail.com
[12/07, 11:18 am] shaileshpatil1996@gmail.com: Adrenal insufficiency could be because of sepsis also sir. But I'm unable to localise here. Her AST/ALT are elevated according to chart . So viral hepatitis ?
Did we send for dengue /malaria ? What about her cue ?
2) It could be even SLE flare sir , as patient stopped taking her steroids abruptly causing both adrenal insufficiency as well as flare .
This confusion between flare and infection always prevails and it's important to differentiate bcoz the treatment is completely different for both
@shaileshpatil1996@gmail.com: send esr and CRP also for her .
And repeat hemogram
Is she giving any symptoms specific for localisation of sepsis. What about her CXR ?
Did someone make elog of current admission with detailed history since she was discharged in june
[12/07, 1:18 pm] Dr Rakesh Biswas Sir: Good questions. @Vinay Gen Med any answers?
I remember there was some Chinese paper shared here earlier that hinted at the efficacy of a particular biomarker to differentiate between lupus flare and bacterial sepsis ? @K vaishnavi mam gen med
[12/07, 1:27 pm] shaileshpatil1996@gmail.com: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5432804/#:~:text=Complement%20levels%20and%20anti%2DdsDNA,disease%20flare%20up%20in%20SLE
Complement levels and anti-dsDNA antibody titer are changed only in SLE with flare, but the changes are usually not considerable at already abnormal levels. Overall, CRP is the most critical marker in differentiating between infection and disease flare up in SLE.
[12/07, 1:32 pm] Dr Rakesh Biswas Sir: Yes Korean Study.
Not a very great study on critical appraisal of the paper last time but anyways what is her CRP?
DIAGNOSIS : Hypoglycemia secondary to ? Adrenal insufficiency with H/O SLE with CNS VASCULITIS
Treatment being given :
IVF NS @ 100 mL / hour .
INJ Methylprednisolone 1gm in 100 mL IV
Inj. Pan 40 mg IV/OD
Inj. Neomol SOS
T.Wysolone 40 mg PO/OD
T.HCQ 200 mg PO/BD
T.Levipil 500mg BD
Oral candid cream
vitals and grbs monitoring




















Comments
Post a Comment